Extremity Compartment Syndrome
exp date isn't null, but text field is
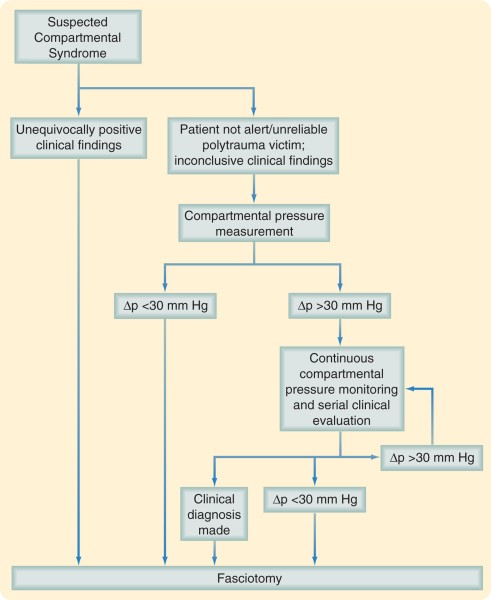
Diagnosis: The diagnosis of acute compartment syndrome requires a high degree of clinical suspicion, a full understanding of the mechanism of injury, and careful serial physical examination.
The presence of distal pulses and the absence of pallor cannot exclude the diagnosis of compartment syndrome because tissue perfusion in a compartment is dependent on both arterial and capillary perfusion gradients. Paralysis and paresthesias are unreliable because studies have shown that peripheral nerves can conduct impulses after 1 hour or more of total ischemic time. Ischemia of muscles, however, causes pain. Patients are typically said to have “pain out of proportion to that expected for the injury.” Unusual requests for frequent narcotic analgesics can be reflective of ischemic pain. Passive stretching of the ischemic muscle of the compartment in question causes exquisite pain and is the most sensitive clinical finding in a developing compartment syndrome. Clinical palpation of the compartment in question plus comparison with the contralateral limb is useful in evaluating a compartment at risk, and any evidence of increased tension or fullness of the compartment should raise clinical suspicion.
Although pain out of proportion to the injury is a cardinal clinical finding of an impending compartment syndrome, it must be emphasized that this pain will diminish as further ischemia occurs. In addition, the clinical findings may be obscured in patients medicated with narcotics, and therefore narcotic administration should be closely monitored.
Systemic hypotension, vascular injury, external limb compression, coagulopathy, and deep venous thrombosis predispose trauma patients to the development of compartment syndrome. In an uncooperative, intoxicated, intubated, or neurologically impaired patient, the diagnosis of compartment syndrome may depend more on measurement of compartment pressures.
Tissue Pressure Measurements
The most common method of measurement is the Stryker Stic device. This hand-held electronic device is easily calibrated and used. Pressures are obtained by inserting the needle into each compartment. It is generally used to make measurements at one point in time and is not an indwelling device.
The highest compartment pressures are usually found at the level of the fracture or within 5 cm of it. Tissue pressure decreased at an increasing distance proximal and distal to the fracture site. It is important to take this into consideration when using the Stryker Stic device to measure compartment pressure in the presence of a long bone fracture.

Compartment Syndrome Algorithm