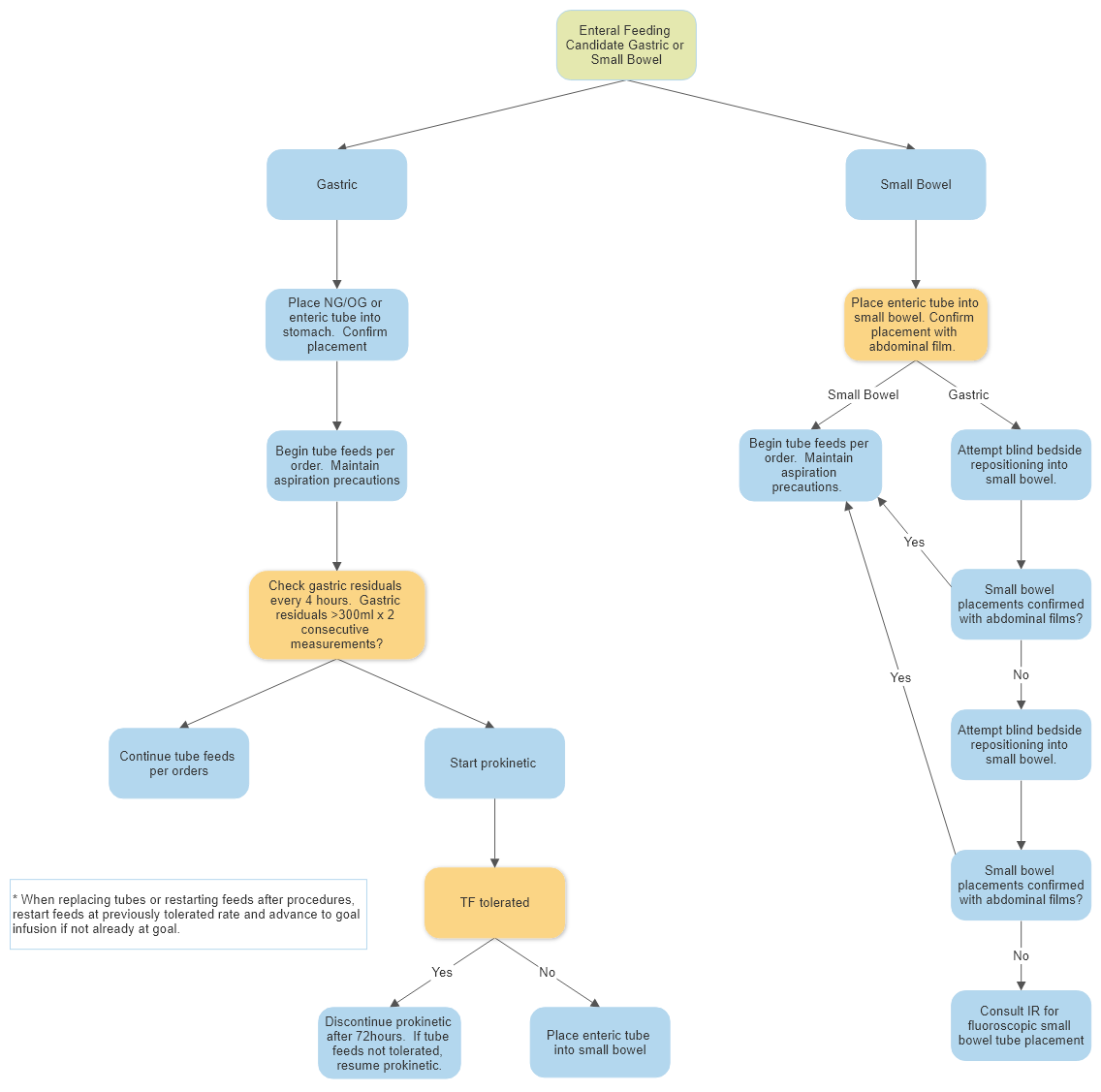
Adult Enteral Feeding Tube Placement Guidelines
exp date isn't null, but text field is
Gastric feeding via an NG or OG tube is acceptable in patients who are at low risk for aspiration. For patients with contraindication to gastric feeding, post-pyloric placement of an enteric tube should be considered (See Section B – Indications for small bowel feeding).
All patients receiving enteral nutrition (EN) must have head of bed elevation ≥ 30 degrees.
- Benefits of gastric feeding:
- Gastric feeds allow for early feeding initiation, ease of tube placement, stress ulcer prophylaxis, and more natural feeding with various feeding options (bolus, gravity, continuous).
- Indications for small bowel feeding: (Not all-inclusive) Enteric Feeding Tube=Small Bore=DHT
- Previous gastric feeding intolerance
- High risk for aspiration (See Section C – Risk factors for aspiration)
- Repeated high gastric residual volumes
- Gastric outlet obstruction
- Proximal Fistula
- Need for multiple operations, procedures and/or tests with plan to feed during procedures (ie. Burn patients)
- Prone position
- NOTE: Although pancreatitis is not an absolute indication for small bowel feeding, post-pyloric feeding tube placement may be considered to improve EN tolerance. Ideal location of feeding tube tip is ≥ 60cm beyond the Ligament of Treitz.
- Risk factors for aspiration: If a patient is at risk for one or more of the following, small bowel feeding tube placement is indicated. Post-pyloric goal is second portion of duodenum or distal.
- Vomiting
- Gastroparesis - If associated with high gastric output*
- History of aspiration
- Medications - Narcotics with high gastric output*
- * When evaluating high gastric output, more than 1 liter /day may indicate small bowel feeding tube placement. If gastric output is between 500ml and 1liter use clinical judgment on whether to proceed with gastric or small bowel feeding.
- Gastric Residual Volumes (GRV):
- Should only be measured in patients receiving gastric feeds
- With one gastric residual measurement > 300ml, if medically feasible, attempt to move patient onto right side for 15-20 minutes before rechecking level
- Ensure patient is having bowel movements
- Prokinetics:
- In the presence of gastric feeding intolerance, gastric motility agents (prokinetics) may be indicated. Special consideration and caution should be used when choosing a prokinetic. Discuss use of any prokinetic with multidisciplinary team.
The use of both Erythromycin and Metoclopramide is more effective than either alone.
Erythromycin 200mg IV q 12 h and Reglan 5 mg IV q 6 h
Nguyen NQ1, Chapman M, Fraser RJ, Bryant LK, Burgstad C, Holloway RH. Prokinetic therapy for feed intolerance in critical illness: one drug or two? Crit Care Med. 2007 Nov;35(11):2561-7
See prokinetic dosing below:
- Erythromycin**: 200mg IV every 12 hours OR oral tablet 250mg every 6 to 8 hrs OR oral suspension 400mg every 6-8 hours
- Metoclopramide (Reglan)***: 10mg IV every 6 hours OR oral 10mg every 6 hrs
For patients with CrCl < 50ml/min, adjust Metoclopramide dose to 5mg every 6hrs
** Erythromycin Drug Interactions: Carbamazepine, Cyclosporine, Theophylline, Aminophylline, Digoxin, oral Anticoagulants, Fluconazole, Amiodarone, Dofetilide, Diltiazem, Voriconazole, Sotalol, Valproic Acid, Haloperidol. Not an all-inclusive list.
*** Extraparamidal side effects have been reported with use of Metoclopramide and patients should be monitored closely.